Medical genetics
Medical genetics
With the increasing availability and complexity of genetic testing, it has become imperative for medical specialists to be fully aware of the limitations and risks included in offering a specific genetic test, as well as the importance of appropriate pre-test and post-test genetic counseling.
Genetic counseling is the stage at which it is evaluated whether a disease condition, actual or potential, is attributable to genetic mechanisms or not, and whether these, possibly, can be defined through specific tests.
The study of genetic diseases not only covers rare diseases, but is also interested in cancers (cancer genetics, especially for breast/ovarian, colon cancers, melanomas, etc.), cardiovascular pathology (e.g., thrombophilia, but also familial hypercholesterolemias, cardiomyopathies, etc.), ENT pathology (hearing impairments, etc.) and ophthalmology(e.g., retinitis).
The consultant geneticist works closely with other specialists to ensure that genetic testing is incorporated into the overall management of patients, ensures that the tests offered are truly indicated and appropriate to high quality standards.
Diagnostic pathways must have procedures to ensure timely reporting and communication of results. As with any medical test, expectations regarding the performance of a genetic test should be discussed with the patient before the test itself is performed (pre-test counseling), allowing patients time to reason about the information they receive and accept or not accept access to it based on truly informed consent. Counseling, both pre-test and post-test, should communicate information in a clear, objective and non-directive manner. In addition to tracking each patient’s personal genetic risk, possible risks to other family members and any children yet to come (reproductive risks) should also be considered and discussed.
A diagnostic definition is not only about the individual accessing the test. Each time it must be determined whether test results involve, and to what extent, blood relatives, because they affect the genetic makeup of an entire family and may affect and be reflected in future generations. The affective, ethical, legal, and social implications of these pathways account for the special delicacy of the doctor-patient relationship in this area.
Thus, the goals of genetic counseling have changed in recent decades: the original goal of preventing birth defects and genetic conditions and the important evolution of technological tools have been complemented by a focus on pursuing the best psychological adjustment by consultees to the information that may be given about a genetic condition or risk involving them and their families. For both goals, it is always stressed that people in counseling, once well informed, should make their own decisions independently, in terms of reproductive and/or with regard to their own life choices or diagnostic and treatment pathways.
Referring specialists
Urology
Urology
Urology is defined as “Branch of medicine concerned with the study and treatment of diseases of the urinary system.”
The treatments that can be performed at Casa di Cura San Rossore are as follows:
- Outpatient services
urological examination - Urodynamic examination (click for more info)
- urinary system ultrasound
- transrectal ultrasound
- scrotal echocolordoppler
- Basal and dynamic penile echocolordoppler
- study with rigiscan
- Day hospital admission to perform a urologic checkup
Referring specialists
Radiotherapy
Radiotherapy
Radiotherapy, within the Casa di Cura San Rossore, represents an activity primarily dedicated to the treatment of cancer and also to the treatment of benign noncancerous conditions. Radiotherapy represents one of the most important cancer treatments and uses high-energy ionizing radiation via special equipment (e.g., linear accelerators) with the intent of destroying the tumor while ensuring maximum attention to the preservation of healthy tissue. The Radiotherapy Unit is staffed by medical, physical, technical and nursing personnel of a high professional level.
MARIA GRAZIA FABRINI
Head of the Radiotherapy Operating Unit.

Graduated in medicine and surgery from the University of Pisa in 1979 with honors, Specialist in Radiology, Radiotherapy and Oncology.
Head from 2002to 2013 of the Section of Brachytherapy and Special Techniques in Radiotherapy at Azienda Ospedaliera Universitaria Pisana, from 2013 to 2015 Director in Charge of Radiotherapy at AOUP.
From 2015 to 2018 Responsible for the Brachytherapy Unit (Interventional Radiotherapy) of the AOUP.
Since 2019 Head of Radiotherapy at Casa di Cura San Rossore.
He has participated in conferences and seminars in Italy and abroad both as a speaker and session moderator.
Author and co-author of numerous scientific publications (see pub med/ google scholar)
He has collaborated with the Tuscan Tumor Institute and Azienda Ospedaliero Universitaria Pisana to develop multidisciplinary pathways for cancer patients.
Adjunct Professor at the School of Specialization in Radiotherapy, University of Pisa
Responsible for radiation therapy (Multidisciplinary Oncology Groups) for gynecological cancers, rare cancers (especially uveal melanoma), upper digestive tract cancers.
Study and research topic integration of radiotherapy with systemic cancer therapies, special and precision techniques in radiotherapy ( IGRT,IMRT, radiosurgery, interventional radiotherapy).
Contacts Secretariat
Ph: +39 050 586130
Fax: 050 586127
Email: radioterapia@sanrossorecura.it
Performance and therapy
Radiotherapy at the Casa di Cura San Rossore has:
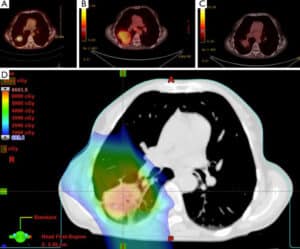
- Computed tomography (Siemens Open Sensation CT), 64 multislice, entirely dedicated to radiation therapy
- TrueBeam STx linear accelerator (see photo gallery above) from Varian Medical System, equipped with an integrated “cone beam CT” device that allows to perform, prior to treatment, a radiological evaluation thanks to which it is possible to monitor the real position of the tumor target and critical organs, correct any positioning errors, and evaluate any displacements even millimeters of the tumor target due to the often non-eliminable movement of internal organs ( organ motion ) and thus irradiate with greater precision.
The TrueBeam STx also has a micro-multilamellar system that allows for high-precision cranial and extracranial stereotactic treatments and, thanks to the machine’s ability to deliver X-radiation even in the FFF (Flattening Filter Free) mode, to decrease the time of dose delivery and thus of the treatment itself
- Treatment planning systems (TPS) used in close collaboration with medical physicists
- Image fusion systems using MiM system for CT, MRI and PET
- Physical-dosimetric instrumentation used for periodic inspection of equipment
- Immobilizers customized according to body district.
Casa di Cura San Rossore also has the following imaging equipment/technology for use in the execution of the treatment plan:
- Internal: Magnetic Resonance Imaging 1.5 Tesla (from San Rossore Nursing Home Radiology)
- External: PET and PET/CT in collaboration with the CNR Nuclear Medicine of Pisa and University Nuclear Medicine of the Azienda Univertsitaria-Ospedaliera S.Chiara of Pisa
This technological equipment then allows us to plan sophisticated radiotherapy treatments such as:
- Volumetric Arc Radiotherapy ( VMAT)
- Intensity Modulated Radiotherapy (IMRT )
- Image-guided radiation therapy (IGRT)
- 3D-CRTconformal Radiotherapy
- Intracranial and extracranial stereotactic radiotherapy (SRS, SBRT)
- Adaptive Radiotherapy (ART)
- Radiotherapy treatments with RESPIRATORY GATING widely used for breast neoplasms, lung etc.
RESPIRATORY GATING technique consists of a treatment in which irradiation is synchronized with the patient’s breathing with the intention of avoiding irradiation of healthy organs close to the tumor.
There are two ways to perform respiratory gating:
- Free Breathing: the patient breathes freely and regularly, and beam delivery is performed in the respiratory phase where the tumor has reduced mobility. The progress of the respiratory cycle is continuously monitored during the treatment so as to make sure that dispensing is done at the correct phase of the cycle.
- Deep inspiration breath hold (DIBH): in which dispensing takes place during the patient’s apnea; for correct apnea amplitude and reproducibility, the patient has both centering and treatment LED displays that provide visual feedback of chest expansion correlated with respiratory movement to help him or her find the correct position immediately (limiting the margin of error due to respiratory movements as much as possible).
RADICAL-CURATIVE:
- As an exclusive therapy:
- treatments with conventional fractionations
- hypofractionated treatments i.e., the ability to deliver high doses with the same or higher therapeutic efficacy thus reducing the overall duration of treatments compared to more traditional schemes
- As combination radiotherapy, integrated in various modalities with surgery (preoperative, intraoperative, postoperative) or in combination with chemotherapy (neoadjuvant, concomitant, sequential), or in combination with hormone therapy or immunotherapy
PALLIATIVE-SYMPTOMATIC:To decrease and/or eliminate symptoms due to neoplastic disease such as pain , compressive syndromes (e.g. mediastinal syndrome, spinal cord compression, etc..) or rarely otherwise uncontrollable bleeding, and/or combined with other therapeutic weapons.
RADIOTHERAPY OF BENEFICIAL LESIONS:For example, pituitary adenomas, meningiomas, arteriovenous malformations (AVMs), Basedow’s disease, keloids, aneurysmal cysts, cranial nerve pathologies (e.g. trigeminal), vascular pathologies.
Clinical evaluation Oncology:
The first contact between the patient and the Center occurs with the first visit to the Radiotherapy Department (“Radiotherapy Oncology Consultation”). During the consultation, the radiation oncology oncologist collects all information, through medical records, about the patient’s current and remote health status to determine the nature and extent of the disease thus proceeding to multidisciplinary consultations.
Once the clinical issue is identified, the radiation oncologist analyzes the possibility of radiation treatment, choosing the most suitable delivery modality for the individual patient, in consultation with colleagues in Medical Physics.
Centering TC:
Upon accepting the patient for radiation therapy, the Radiation Oncologist and the Medical Radiology Health Technician (TSRM) perform a centering CT scan by defining the patient’s position on the couch and determining the type of immobilization system best suited for the type of therapy to be delivered.

Contornation:
Next, the radiation oncologist identifies the sensitive structures to be contoured on the centering CT scan. To do this it also uses information from other diagnostic investigations such as MRI and PET. Thanks to modern software in the Center, the radiation oncologist has the ability to “fuse” all the patient’s diagnostic images, managing to pinpoint with millimeter precision the region to be irradiated.
Development of the treatment plan:
The Medical Physicist prepares the Treatment Plan by optimizing the dose in the target volume while trying to spare the healthy organs surrounding the disease as much as possible. Each patient will therefore have a Care Plan that is strictly individualized, and suitable for achieving the most accurate dose distribution; consequently it will be different from that of any other patient. After the planning is finished, the Medical Physicist presents the plan to the Radiation Oncologist, which will be analyzed, discussed, possibly modified, and accepted.

Before being dispensed on the patient, the Plan is verified on the ArcCheck dummy (for verification of rotational treatments) by evaluating its correct dose delivery (step in the overall Quality Control pathway)
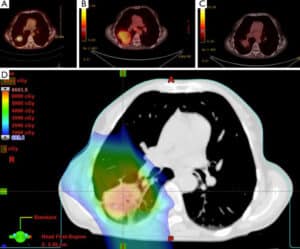
Verification of positioning and treatment:
To carry out the treatment session, the patient is introduced inside the room (Bunker) where the linear accelerator is housed and is made to lie on the treatment couch. A CT scan is taken of the region to be irradiated before radiation is delivered and compared with the centering CT scan. With this procedure, it is possible to position the patient with millimeter precision.
The patient inside the therapy room is constantly monitored by the TSRM through a closed-circuit video system. In addition, an intercom system via intercom allows the patient to communicate with the technician. Throughout the radiotherapy treatment, the Patient will undergo follow-up visits during which any supportive therapy will be prescribed. Periodic follow-up visits are carried out after the conclusion of treatment.

Radiation treatment is performed either on an outpatient basis or on an inpatient or day-hospital basis for special clinical cases or for ‘performing combination therapies ( e.g., chemotherapy, nutrition, supportive medical therapy). Admission to ward or dedicated housing is also possible for special logistical situations (Click here to browse our solutions for your stay)
Radiation Therapy collaborates both within the Casa di Cura within dedicated Multidisciplinary Groups and with the various specialists at other National Centers for the discussion of the most complex clinical cases to ensure that each patient receives the proper integration and personalization of planned treatments based on international protocols and guidelines interior adapted to the clinical situation of each individual patient.
The Physician verifies and evaluates all the parameters of your treatment plan, verifies every radiological image performed before and during treatment including by Cone Beam verifications at the time of treatment for correctness of therapy; performs intercura
The medical physicist:
It ensures through periodic checks that the characteristics of the equipment are within the tolerance levels chosen to ensure the optimal performance of treatments. It ensures the treatment pathway: from the preparation of the treatment plan, to its approval following discussion with the physician, from the transfer of the plan to the treatment machine through the Record and Verify (ARIA) system that allows the identification of the patient, the correct association of his or her treatment plan and the recording of the dose delivered to each fraction, to the verification before the start of the treatment of the correct delivery of the plan by the equipment and also supervises with other working figures (physicians and technicians) during treatments with respiratory gating.
The TSRM health technician:
Works according to the instructions of the radiation oncologist at the various stages of the radiation therapy procedure: performs patient set up, if necessary using positioning and immobilization systems; during the simulation phase of the treatment, acquires the images necessary for the production of the treatment plan and prepares the accessories necessary for its implementation (shielding, etc.); performs the radiation treatment according to the indications of the plan prepared and approved by the physicist and physician and is responsible for the correct application of the plan itself; acquires the images produced with IGRT technology and assists the radiation oncologist in the “on line” control for the correction of the set up. Prior to the start of treatment carry out the check together with the physicist of the correct delivery of the plan by the machine.



Referring specialists
Rheumatology
Rheumatology
Rheumatology deals with all acute and chronic diseases of the joints, such as:
- arthrosis
- rheumatoid arthritis
- Psoriatic arthritis
- spondylitis
- connective disorders, such as systemic lupus erythematosus, scleroderma, Sjogren’s syndrome, polymyositis and vasculitis
- Fibromyalgia and muscle rheumatism
- Regional joint diseases, such as scapulohumeral periarthritis, carpal tunnel syndrome, etc.
Diagnostic insights include blood chemistry tests, serology for autoimmune diseases, radiology, and ultrasound, depending on the diseases involved.
Referring specialists
Senology
Senology
Senology is a complex of instrumental investigations (mammography with tomosynthesis, digital mammography, ultrasound, MRI, interventional procedures under ultrasound guidance, stereotactic radio-guided), which are used in the study of breast pathology.
These investigations are applied both in the control of the asymptomatic patient and in the verification of the symptomatic patient. In the first case as prevention in the belief that early diagnosis is the first solution to breast problems; in the second case in the belief that preoperative diagnosis and staging is the first solution to the intercourse problem.
In Tuscany, in Pisa, the Casa di Cura San Rossore represents a center of excellence for breast diagnostics.
Methods
Casa di Cura San Rossore has a wide range of applications to improve diagnostic confidence and to properly plan the diagnostic/therapeutic course in surgical patients. Department Specialists also provide ongoing support from prevention to follow-up.
Activities
A team of professionals with multi-specialty expertise, state-of-the-art machinery and interdisciplinary collaboration enable the symptomatic and non-symptomatic patient to receive personalized diagnosis and treatment at the Casa di Cura San Rossore.
The patient (or the patient since breast pathology also affects the male sex) is thus accompanied step by step through the diagnostic and then therapeutic pathway. A humanized path that takes into account the specifics of each case and is followed at all stages: from radiology to cytopathology, from molecular diagnostics to radiation therapy, from cancer surgery to plastic surgery, and ending with rehabilitation and psychological support.
The Breast Diagnostic Center of the Casa di Cura San Rossore performs: Inpatient Activities The type of malignant pathology generally allows for short hospitalization preceded by some pre-operative examinations. For this purpose, the facility has rooms equipped with one or two beds, each specially furnished to ensure the best possible environmental and care comfort during hospitalization. In addition to the normal facilities, each room is also equipped with: self-contained toilet facilities, adjustable bed with hand control by electronic control, hand control with microphone, telephone, TV equipped with Sky service and satellite channels, Internet connection, air conditioning, safe. Some wards then have a sitting room and an adjoining room for a possible companion. For more information, the Admissions Office can be contacted at +39 050 586336.
Day-Surgery Activities
Benign pathology, where the patient’s condition permits, is addressed under Day-Surgery. For more information you can contact the Admissions Office at +39 050 586336
Outpatient Activities
Examinations for patients with established or presumed breast pathology are conducted in the outpatient clinic. For more information you can contact the Secretariat at +39 050 586217
Secretariat
For more information, you can contact the Secretariat at +39 050 586432 from 9:00 AM to 1:00 PM or send an email to the following address: senologia@sanrossorecura.it
Fields of action
Diagnostic senology, as a methodological approach to breast cancer diagnosis, involves the following:
- Routine breast monitoring of asymptomatic patients
- Breast check of symptomatic patients for mastodynia, relief of palpable lesions, skin changes (redness-retraction), asymmetry.
- Organization of the individualized breast pathway by age, by pathology, by risk factors (family history, previous pathology)
- control patients at risk (BRCA)
- control oncology patients
- Interventional in focal pathology
- Counseling on previously performed and inconclusive imaging and examinations
- Guidance in the management of the diagnostic/therapeutic process (follow-up, surgical evaluation)
Performance and therapy
Mammography with tomosynthesis, also known as 3-dimensional mammography, is an innovative 3-D technique that reduces the number of false negatives compared with examinations performed with a 2-D technique.
3D mammography represents a high-definition three-dimensional version of digital mammography.
The new mammography, also known as digital breast tomosynthesis, represents a breakthrough in diagnostics: the basic principle is the same as tomography: it makes use of images captured from different angles, with reconstructions of volumetric figures, thus enabling the physician to detect any abnormalities or pathologies that would otherwise be undetectable.
In practice, unlike a normal mammogram, where the machine is fixed, in tomosynthesis the instrumentation moves around the breast. Volumetric reconstruction, in principle, makes it possible to overcome one of the main limitations of two-dimensional imaging and thus of radiological imaging (digital mammography) currently in use, namely the masking of lesions (masses, microcalcifications, distortions, etc.) caused by the superimposition of normal structures. This situation occurs most often in young patients with radiologically dense breasts. The advantage of this is that it is easier to find any hidden tumor tissue.
The opportunity, in fact, to dissociate different planes by tomosynthesis makes it seem possible to reduce the number of false negatives and false positives, due to the overlap, allowing a substantial improvement in the detection and analysis of lesions: conviction of their presence and certainty of their absence.
Digital mammography is a diagnostic method that uses equipment called a digital mammograph to form the mammographic image.
In digital mammography, the X-ray film is replaced by a detector: this absorbs X-rays transmitted through the breast and converts their energy into electronic signals, which are digitized and fixed in computer memory. An image, the digital mammogram, is then derived from this set of data and displayed on a high-definition monitor. From there, after being properly processed, it can be imprinted on film using a laser printer or stored in one of the various storage systems available today, including CD-ROM.
It lasts a few minutes and no drugs are administered or contrast medium used. Mammography is the most effective and safe means of early detection of breast cancer. In fact, it helps to detect small changes in the breast before other signs or symptoms appear. If such changes are noticed early, there is a very good chance of full recovery.
Advantages:
- Optimization of ionizing radiation dose
- Image modifiability by processing
- Display on monitor and on film
- Digital archiving: exams remain stored within facility computers for later comparison
- Remote transmission
Ultrasound is a method that uses ultrasound that is sound waves of frequencies above 20,000 Hz that are inaudible to the human ear. This makes the examination harmless and repeatable. Ultrasound equipment uses probes, called transducers, that emit ultrasound beams that pass through the various tissues of the human body and generate reflected beams that return to the transducer and are called return echoes. In senology, ultrasonography effectively accompanies and complements the mammographic examination and, above all, represents a supplement to the clinical examination (breast examination) , which no longer has any reason to exist without instrumental support such as ultrasonography that makes immediately visible what is manifested by palpation. Ultrasound is the investigation of first choice in women younger than 40 years of age, in whom the still predominantly glandular structure of the breast does not make study by mammography effective. The periodicity of the ultrasound examination is decided by the radiologist on the basis of the patients’ registry age, family history (presence of relatives with breast cancer disease), pathological history, current or previous hormone therapy, and mammary gland structure.
Advantages:
- High frequency 10-13 MHz probes with high image definition
- State-of-the-art ultrasound machine
- Software dedicated to breast study
- Echocolordoppler study
Mammary Magnetic Resonance Imaging (MRI), introduced in the early 1990s, has definitely entered the clinical mainstream to complement the traditional breast diagnostic techniques represented by mammography and ultrasonography. MRI examination of the breast, in addition to the morphological investigation of breast lesions, allows the functional evaluation of breast lesions by assessing their vascularity, which appears different in healthy and pathological tissues. The examination can be performed with or without the use of paramagnetic contrast medium, depending on specific clinical indications.
The use of contrast medium, which has intravascular and interstitial distribution, in MRI enables the identification of breast cancer, as it markedly increases its signal intensity compared with surrounding tissues.
Contrast-free breast MRI has as its main indication the study of prosthetic implants, particularly in the evaluation of integrity and possible complications, both for prostheses applied for cosmetic purposes and for reconstructions after oncological surgeries.
The indications of breast MRI with contrast medium are as follows:
- Screening in young women with genetic risk or high familial risk for breast cancer
- Search for primary tumor in case of metastasis of unknown origin to probable breast site with clinical breast examination, mammography and ultrasonography normal (CUP SYNDROM)
- Local staging of malignancies already diagnosed by conventional techniques.
- Control of breast cancer response to neoadjuvant chemotherapy.
- Evaluation of breast operated women when mammography and ultrasound cannot differentiate scar from tumor recurrence.
- Study of breasts with implants.
- Disagreement between mammography images, ultrasound images, and clinical examination.
- Secreting udder.
This examination cannot be performed in case of:
- Presence of pace maker;
- Presence of ferrous metal prostheses.
IMPORTANT INFORMATION FOR USERS
The detection of doubtful and/or suspicious lesions results in the need for histological characterization, which is a key step in the patient’s subsequent course of action.
The stereotactic tomosynthesis IMS biopsy is performed in the prone position, in clinostatism (lying down), and allows localization and guided RX retrievals of otherwise unreachable findings.
The finding obtained by tomosynthesis biopsy is the same as that detected by 3D mammography, which is otherwise not always detectable by the 2D technique, due to the masking phenomenon discussed above. It is therefore a rapid biopsy procedure devoid of the discomfort inherent in sitting biopsy and therefore better tolerated by women.
With this system, the lesion can be reached from various angles, and the layer of interest is brought into focus.
The innovation present at the Casa di Cura San Rossore in Pisa, a center of excellence in Tuscany, consists precisely in the prone position, the rapidity of the examination and the lower dose of ionizing radiation administered during the examination.
A breast interventional procedure is defined as any minimally invasive act performed on the mammary gland that is intended to condition the subsequent diagnostic or therapeutic course. The choice of the best method is customized by the radiologist based on the characteristics of the pathological finding, its size, and the method by which that finding is best visualized.
Radioguided interventional, mammotome
- Indicated for histological typing of microcalcifications, opacities, distortions and otherwise lesions visible on mammography.
- Computerized guide for withdrawal
- Microhistological sampling with forced aspiration (mammotome) resulting in an abundance of material
- Unlike many other centers where such a procedure is done in the sitting position, stereotactic biopsy at Casa di Cura San Rossore is performed with the patient lying down, prone: clinostatism, that is, the lying position, greatly reduces the discomfort of the procedure compared to the sitting
- Local anesthesia
- Localization of non-palpable lesions
Echoguided interventional
- Indicated in cytohistological typing of lesions visible on ultrasound
- Real-time ultrasound guidance at needle introduction for continuous verification of correct sampling.
- Thin needle: cytological sampling
- Tru-Cut/Mammotome: microhistological sampling
- Local anesthesia
- Speed of execution
- Presurgical localization of non-palpable lesions
Sexology
Sexology
The Clinical Sexologist is a psychologist, specializing in clinical sexology, who deals with the sexual health of men and women: counseling, diagnosis, and treatment of male and female sexual dysfunction.
The clinical intervention of the clinical sexologist is based first on an accurate psychosexological history and diagnosis, and then provides, once the specific problem of the patient or couple has been identified, tasks for the couple to perform at home that will allow them to become familiar with their own corporeality and their affective, emotional, and psychological experiences related to pleasure, intimacy, involvement, and sexual arousal.
Services offered:
- Sex counseling
- Individual sex therapy
- Couples sex therapy
- Treatment of male sexual dysfunction
- Treating female sexual dysfunction
- Support for MAP (Medically Assisted Procreation)
Referring specialists
Pain therapy
Pain therapy
Pain Therapy at Casa di Cura San Rossore provides the following outpatient activities:
- lumbago and low back pain treatment(peridural infiltration and caudal block,ecoguided facet joint block)
- cervicobrachialgia treatment
- Headache treatment (including prevention by use of Botulinum Toxin)
- Trigeminal neuralgia treatment and herpes zooster
- Fibromyalgia treatment and myofascial syndromes
- Echoguided joint and periarticular infiltrations
- Neuropathic pain in diabetic neuropathy
- Pain in lower limb ischemia
- Echoguided intercostal and paravertebral block in chest pain
- Botulinum Toxin infiltrations (chronic migraine prophylaxis,muscle pain,piriformis syndrome,epicondylitis)
- Percutaneous radiofrequency electrical neuromodulation treatments
- Spinal cord and peripheral neurostimulation implants
Referring specialists
Internal medicine
Internal medicine
Internal Medicine is the branch of Medicine that deals with the diagnosis, medical treatment and prevention of diseases and disorders of the internal structures of the human body (Dorland). The goal of Internal Medicine is also to coordinate in the patient, evaluating the patient as a whole, the specialized diagnoses and therapies of the internal organs and systems. The internist has the theoretical, scientific, and professional knowledge in the fields of medical pathophysiology, functional and instrumental medical semiotics, clinical methodology, evidence-based medicine, general medical clinic, and medical therapy.
Casa di Cura San Rossore has the most modern hematochemical and instrumental diagnostic means, which, used by specific specialists working in the facility, allow all kinds of diagnoses to be made.
When required, the Internal Medicine service of the Treatment Center is able to collaborate with all specialists, both medical and surgical, for the comprehensive evaluation of the patient.
Referring specialists
Regenerative medicine and PRP (Platelet Rich Plasma)
Regenerative Medicine and PRP
The Center for Regenerative Medicine at Casa di Cura San Rossore aims to bring therapeutic benefit to patients through the use of platelet-rich plasma (PRP).
The Casa di Cura San Rossore is authorized by the Region of Tuscany to practice infiltration with blood components.
What is PRP?
PRP (Platelet Rich Plasma) is a powerful concentrate of Growth Factors that stimulates tissue regeneration and the growth of new blood vessels.
Growth factors, contained in platelets circulating in our blood, activate biological mechanisms such as direct cell migration (chemotaxis), cell proliferation, and cell differentiation, which are key events in tissue repair and regeneration processes.
It has been observed that the concentration of growth factors contained in PRP activates certain biological functions by promoting regeneration the repair of bone and other soft tissues in the treated areas.
Scientific studies have shown how locally administered PRP activates and accelerates connective tissue repair processes: tendon and muscle injuries, chondral or osteochondral injuries, meniscal injuries.
Pain and mobility are improved by the combination of biocompatible scaffolds combined with the cell-stimulating properties and anti-inflammatory action of PRP-released growth factors.
The fields of application of PRP:
Traumatology and Orthopedics
Sports Medicine
Dermatology and Trichology
Ophthalmology
Dermatology
Dentistry
Plastic Surgery
Maxillofacial surgery
Anti-Aging
Gynecology
Urology
The clinical benefits of PRP:
No side effects such as allergies or intolerances;
Stimulation of reparative processes and growth of injured tissues;
Since the patient’s own blood is used, there are no communicable diseases.
Nephrology
WORK IN PROGRESS
Page under construction
For information contact +39 050 586217 or send e-mail to info@sanrossorecura.it